In a healthcare environment increasingly focused on value-based care, the need for proactive, patient-centered solutions has never been greater. Yet, much of the system still emphasizes treating illness after it arises—rather than preventing it in the first place. The result? Rising costs, overburdened emergency rooms, and patients falling through the cracks.
At the heart of the solution lies Advanced Primary Care Management (APCM) — a comprehensive care model that does more than treat symptoms. It anticipates needs, supports long-term outcomes, and reshapes how we think about prevention.
The Problem with Reactive Care
Reactive care dominates most clinical settings today. While it can effectively address immediate issues, it often fails to prevent the escalation of chronic conditions.
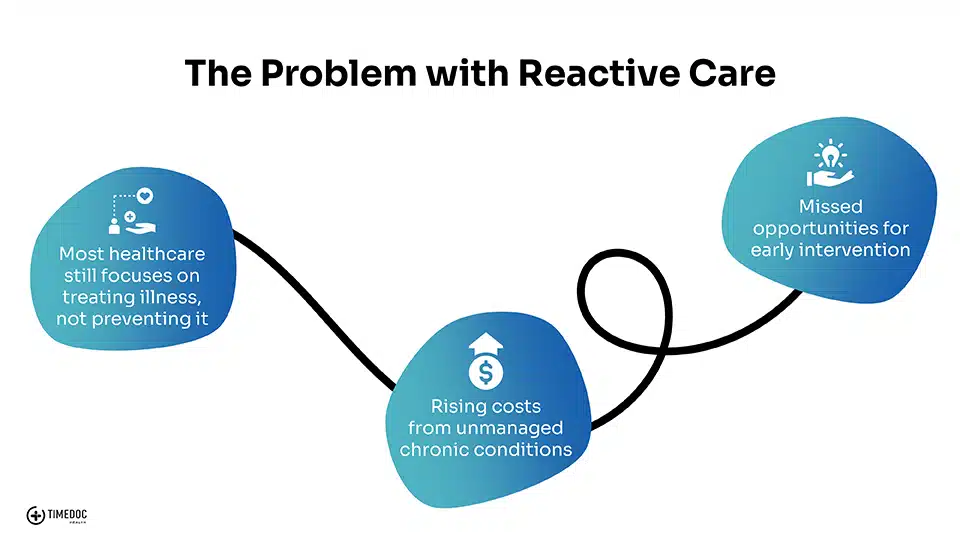
The consequences are significant:
- Escalating healthcare costs from unmanaged chronic illnesses like diabetes, heart disease, and COPD
- Missed opportunities for early intervention, leading to avoidable hospitalizations
- Over-reliance on emergency departments for issues that could have been resolved earlier
In underserved and high-risk populations, these challenges are compounded by limited access to care and complex social determinants of health.
What is APCM – and Why It Matters
Advanced Primary Care Management (APCM) is a modern, evidence-based model that brings together multiple proactive services under one umbrella.
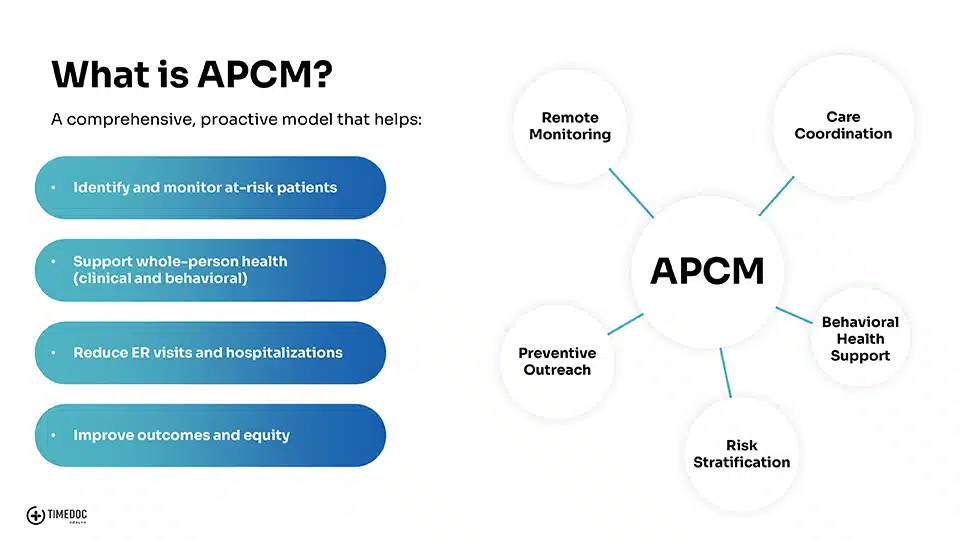
Unlike traditional care approaches, APCM helps providers stay ahead of health issues by integrating:
- Risk Stratification: Identifying patients who need the most attention
- Remote Monitoring: Capturing real-time health data to prevent deterioration
- Care Coordination: Ensuring smooth communication and follow-through across the care team
- Behavioral Health Support: Addressing mental and emotional health as part of whole-person care
- Preventive Outreach: Regular check-ins and health coaching to reinforce preventive habits
Together, these components allow providers to offer consistent, high-touch support that improves both outcomes and patient satisfaction.
Why APCM Should Be Recognized as Preventive Care
Today, many APCM services are still classified as chronic care or follow-up care. But reframing APCM as preventive care isn’t just a matter of semantics—it’s a catalyst for improving access and impact.
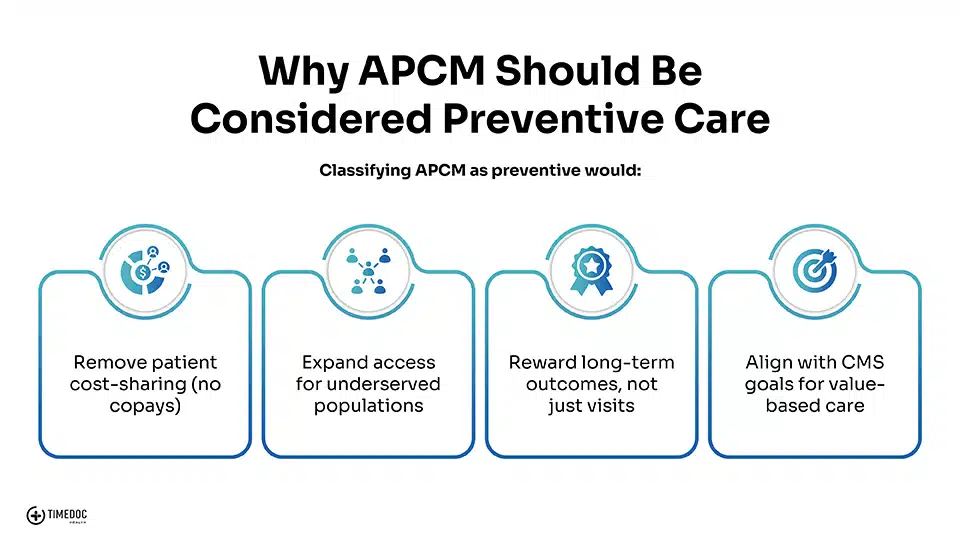
Reclassifying APCM would:
- Eliminate patient cost-sharing, removing financial barriers to participation
- Expand access to underserved populations, who are most impacted by gaps in preventive services
- Reward long-term health improvements rather than visit-based reimbursement
- Align with CMS’s goals for value-based care and population health management
Prevention is more than vaccines and annual checkups—it’s consistent engagement, early risk detection, and ongoing support. APCM fits squarely into that definition.
How TimeDoc Health Powers APCM
At TimeDoc Health, we provide the infrastructure, people, and technology to bring APCM to life across your organization.
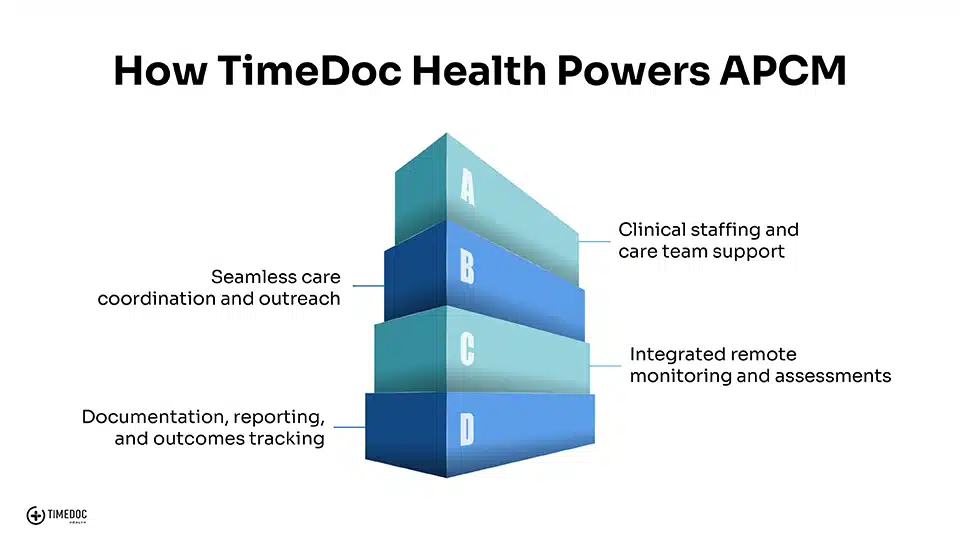
Here’s how we do it:
- Clinical Staffing: Supplement your team with dedicated care coordinators and clinical staff
- Seamless Care Coordination: Keep every stakeholder informed with centralized communication and task management
- Remote Monitoring & Assessments: Monitor vital health data remotely with real-time insights and alerts
- Reporting & Documentation: Ensure compliance and measure impact through streamlined documentation and outcomes tracking
Whether you’re just getting started with population health or scaling an existing program, TimeDoc Health helps you deliver proactive, personalized care at scale.




