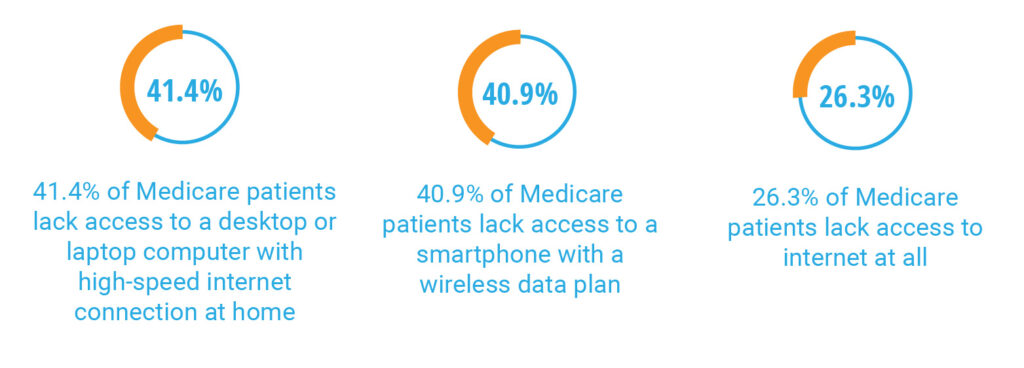
With limited doses available in the first phase of vaccination, the demand to provide this life-saving immunization to our elderly population far outweighs the current supply. And whether health centers are self-administering the vaccine or referring patients offsite, one thing has become increasingly evident: our healthcare system is set up to favor vaccination for those who are tech-literate with access to the internet, leaving behind everyone who falls outside of these criteria. Mass vaccination’s frenzy demands elderly Americans to figure out the entire process themselves. It starts with the requirement of using web-based appointment scheduling applications to secure an appointment successfully. While this prerequisite may appear to be small, it necessitates technology-enabled devices and reliable access to the internet, two unequally distributed resources. The issue becomes apparent when we uncover that many Medicare patients, especially those who are dual-eligible, do not have internet-compatible devices, let alone access to broadband itself. In fact, according to a recent study in response to the COVID-19 pandemic conducted by University of Pittsburgh and Harvard University researchers, it was found that:
Technology Access Continues to Be a Struggle For Medicare Patients
Here is an even harder truth: for adults 65+ that have adequate internet access, only 27% feel confident using smartphones, computers, or other electronics to complete necessary tasks online*, proving that familiarity of technology use also plays a role. The implications of these metrics vividly illustrate the unfortunate digital disparities among the at-risk population that hinder them from receiving proper care. So many patients lack access to or comfort using technology to acquire an appointment that our health system may very easily overlook the population that is undoubtedly the most in need of the coronavirus vaccine.
What This Means For Health Centers
Health centers must bear the responsibility on their shoulders to guarantee their vulnerable patients do not get left behind. Ambiguity still exists around which clinics will self-administer versus send patients offsite, but despite the route that gets determined, patients with digital disparities need proactive guidance and support to navigate them through the intricacies of their vaccine journey. In the current environment, Medicare patients, especially dual eligibles, are feeling overwhelmed and confused and are turning to their primary care providers for help addressing the hurdles related to COVID-19 immunization. This greatly impacts Federally Qualified Health Centers(FQHCs) and Rural Health Clinics(RHCs), who exist for the purpose of improving health equity among the underserved. At the end of the day, Medicare beneficiaries need assistance addressing the communal challenges they face surrounding vaccine coordination. Health centers can help improve upon the immunization process for their at-risk patient population rather than relying on them to seek guidance elsewhere.
What Should Health Centers Do Now
With over 91% of the 65+ population having access to a cell phone**, telephonic outreach needs to be utilized to address the gaps caused by digital access.
Community health centers must act now to integrate proactive, phone-based outreach to vaccine eligible patients in preparation for the vaccine. Early engagement with underserved, Medicare patients can ensure they have a spot in line as vaccine distribution starts to extend across the country. Telephonic outreach not only helps health centers break the barriers of appointment scheduling, but also aids in the many steps needed in the process to full vaccination. Between pre-appointment preparation through post-vaccine follow up with the second dose, phone based patient outreach seeks to uncover and address the challenges patients face throughout their vaccination journey. Such challenges can include:
- Coordinating Vaccinations: Medicare patients are not able to figure their questions and concerns without speaking to a live person, these patients need someone to help them understand the process while coordinating the necessary steps to achieve vaccination.
- Transportation: Issues with transportation are particularly present for patients that will be directed to off site vaccination. Self-travel by car is rarely an option for elderly patients and public transit can be limited in certain areas. Outreach seeks to ensure that patient’s transportation needs are met.
- Special Needs: Homebound seniors with vision, hearing and mobility impairments require additional attention, especially when they are directed towards mass-vaccination sites (such as stadiums or churches) that pose additional accessibility challenges.
- Language Barriers: Minority seniors are further disadvantaged due to language barriers and require added efforts to navigate them through the elaborate process.
While the end of this monumental health crisis may seem to be in sight, it is essential for health centers to act now. Many FQHCs are taking a hands off approach due to a lack of capacity and are passively referring their patients to vaccine sites in their community. While the lack of staffing capacity is understandable, this passive approach is not enough to keep Medicare patients, and especially dual eligibles, from slipping through the cracks. Whether health centers are administering the vaccine onsite or not, patients need proactive, telephonic outreach from their clinic to help them get immunized. Available data shows us that people with chronic conditions are much more likely to have severe reactions to the coronavirus. With more than two-thirds of Medicare beneficiaries suffering from chronic conditions, a fundamental shift in the approach to handling the coronavirus vaccine is needed. Patients need help now and even if organizations are not scheduled to receive their vaccines until a later date, they must take advantage of this time to reduce the disparities in digital access. Unfortunately, the unequal distribution of technology is abundantly clear, but health centers can contribute to reducing the disproportionate toll it takes on the underserved Medicare population. Where digital disparities seem to be the cause in delaying clinical intervention, telephone-based engagement can emerge as the leading solution for health centers to proactively bring health equity to individuals 65 and older.

