
The healthcare industry is facing a growing challenge.
In the aftermath of the COVID-19 pandemic, providers are still stretched thin, facing staffing shortages and burnout, struggling to offer effective support for people with chronic conditions. And unfortunately, there’s a lot of them: six in ten Americans live with at least one chronic disease like heart disease, cancer, or diabetes. The CDC also reports that these and other chronic diseases are the leading causes of death and disability in America, and are the leading drivers of the nation’s $4.1 trillion in annual health care costs.
With such a major challenge, how can providers possibly begin to address these issues? Remote patient monitoring programs, while not a silver bullet, are gaining popularity due to their effectiveness in addressing patients with chronic conditions. But how does remote patient monitoring work? Is it worth the cost of implementation? What are the potential downsides of these programs?
At TimeDoc Health, we’re here to answer all these questions and more. We’ve put together this guide to remote patient monitoring to help you gain a base of knowledge about these important initiatives and the technology that supports them. Let’s get started.

What is remote patient monitoring?
Remote patient monitoring (RPM), is a beneficial healthcare approach designed to keep doctors connected with their patients’ health status, regardless of the distance between them. It typically involves the use of digital technologies to collect health data from patients in one location and then electronically transmit the information securely to healthcare providers for assessment and recommendations.
The term “remote patient monitoring” is a term that can have many definitions—RPM can also be referred to as remote physiologic monitoring, since you’re monitoring how each patient’s organs function normally. In fact, Medicare uses the term “remote physiologic monitoring” in their coding and billing language. For Medicare, RPM is a set of codes that describes non-face-to-face monitoring and analysis of physiologic factors used to understand a patient’s health status.
At the heart of RPM are devices that are easy to use and designed to monitor a range of health metrics like blood pressure or weight. Collecting this physiological data is just the first step—what really matters is what you do with the information—more on this in a moment.

The Benefits of Remote Health Monitoring Services
RPM enables a continuous loop of monitoring that helps shift the paradigm from reactive care to proactive care. Ultimately, the impact of RPM includes:
- Patient Engagement and Empowerment: RPM engages patients by providing them with the tools to actively monitor their health. This approach helps individuals understand their conditions better and fosters a sense of control over their health outcomes.
- Early Detection and Prevention: With continuous monitoring, providers are able to establish a baseline and set alerts if symptoms fall outside of the normal range. By catching abnormal symptoms early, healthcare providers can intervene sooner, preventing conditions from worsening.
- Reduced Hospitalizations and Emergency Visits: Due to early interventions, patients can often manage their condition effectively at home. This can lead to fewer hospital stays and emergency visits, ultimately improving patient quality of life and reducing healthcare costs for both patients and providers.
- Improved Medication Compliance: RPM can improve medication adherence by reminding patients to take their medicine and allowing providers to check if treatments are followed correctly through data monitoring.
- Optimized Resource Allocation: By understanding who needs immediate attention through real-time data, providers can allocate resources more efficiently, enhancing the overall quality of care.

Types of Remote Patient Monitoring Devices
Three of the most common types of RPM devices are blood pressure devices, scales, and blood glucose meters. These three devices are commonly used to manage and monitor chronic conditions, connected via bluetooth or cellular to transmit data to the provider, enabling proactive management of patient health.
Blood Pressure Devices
RPM blood pressure devices enable patients to take regular measurements at home, a vital process for people dealing with conditions like hypertension. The routine flow of data from patient to provider gives the opportunity for immediate interventions if readings fall outside of the patient’s target range, aiding in medication or lifestyle changes to better control high blood pressure.
Scales for Weight Management
The scales used in RPM play a vital role in managing and monitoring conditions like heart disease, obesity, and fluid retention. By providing accurate and timely weight data, these scales help healthcare professionals identify trends, make adjustments to treatment plans, and offer dietary or lifestyle advice to manage weight effectively.
Blood Glucose Meters
Often used by individuals managing diabetes, cellular-enabled blood glucose meters allow for the direct transmission of blood sugar readings to health care providers. This real-time data sharing can help you adjust medications and dietary recommendations in order to maintain optimal glucose levels.
How Do I Set Up Remote Patient Monitoring for My Practice?
Especially with the right software, setting up an effective remote patient monitoring system is probably less complicated than you think. Here’s how TimeDoc Health collaborates with providers to design and implement a successful RPM program, in 5 steps:
1. Kickoff:
This step is all about learning your needs and setting clear expectations and objectives for the remote monitoring program. We know that a successful RPM program requires communication and collaboration, as well as effective software—and TimeDoc Health provides all three. Especially with a finite budget to consider, getting your program up and running (and delivering ROI) in a timely manner can make or break the initiative.
2. Implementation
With the foundation set and the RPM program’s scope defined (including which conditions and/or patients to initially implement RPM with), implementation can begin. This includes the provision of RPM devices as well as determining clear workflows for configuring these devices and monitoring their readings. This may include working with APIs to enable seamless integrations with EHR and related systems.
3. Enrollment
In most cases, we recommend working with an experienced RPM partner like TimeDoc Health to help you with the roll-out of your RPM program. In addition to thinking about condition- or device-based RPM implementation, you should also consider Medicare enrollment since it covers around 80% of the cost of remote patient monitoring in the U.S. As you enroll patients, you can introduce them to RPM and set expectations for how they should use their RPM device(s).
4. Care Coordination
At this stage, RPM officially begins. From the comfort of their homes, patients can begin taking readings with their RPM device(s) as advised by their provider. Meanwhile, provider organizations can set up the workflows and dashboards associated with their side of RPM, so they can efficiently monitor their patients’ readings and know when to intervene.
5. Documentation
All the health data in the world is virtually meaningless if it’s not accessible and actionable. With TimeDoc Health’s remote monitoring solution, readings are automatically transmitted, and custom integrations can be set up to sync this data with other systems and applications, including EHR integrations.
Remote Patient Monitoring Software
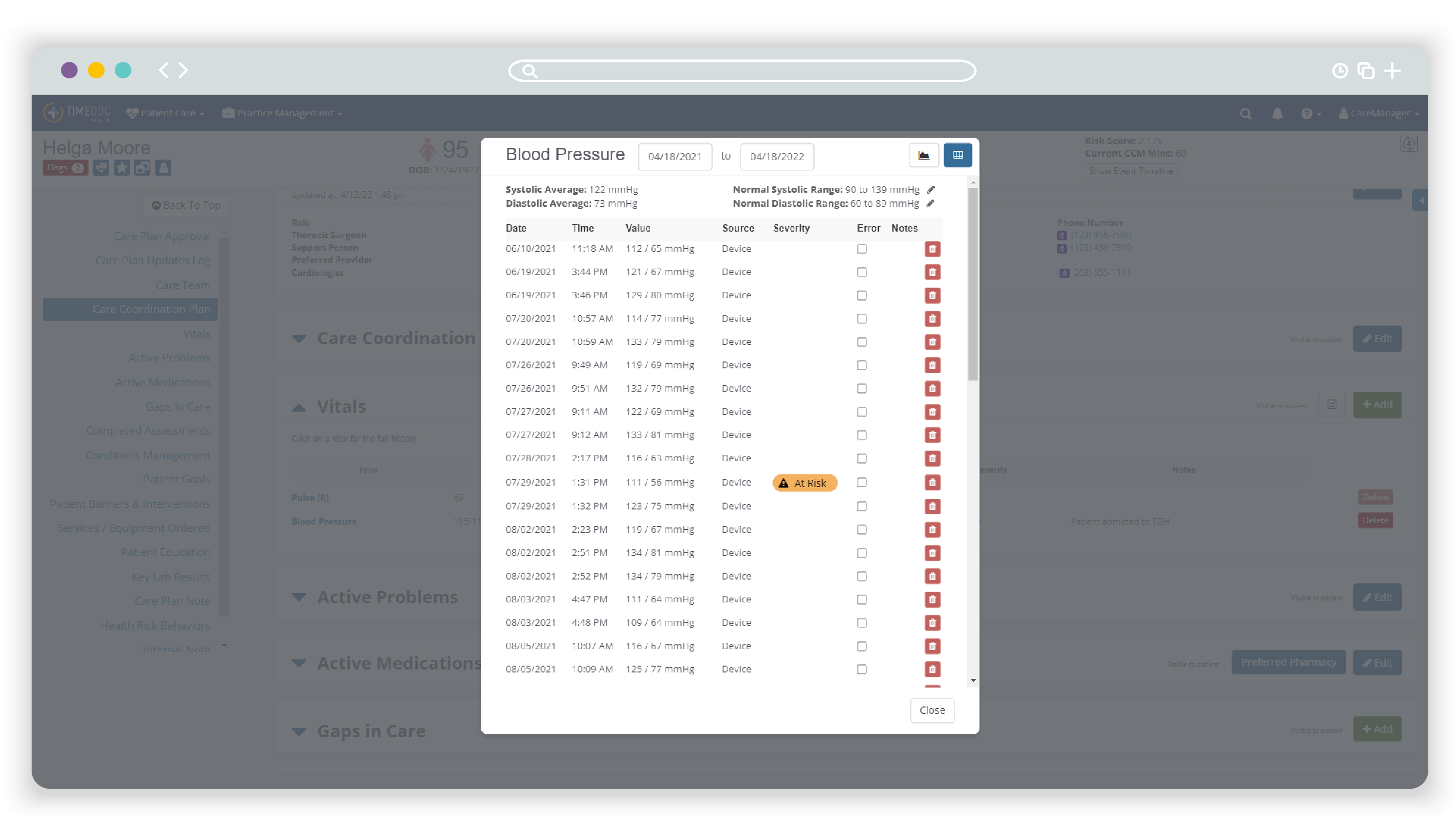
Remote patient monitoring software is any type of technology platform that healthcare providers use to collect and analyze the data that patients submit from their devices at home. At TimeDoc Health, our RPM platform is a prime example of advanced RPM software, designed to integrate seamlessly with existing EHRs. Aside from the collection and transmission of health data between patient and provider, the TimeDoc Health platform plays a crucial role in allowing you to do something with the data you receive.
Our real-time data analytics capabilities trends patient vitals over time and generates alerts for healthcare providers when readings fall outside of a patient’s predefined safe range. This functionality gives you the ability to make data-driven decisions, intervening as necessary to address potential health issues before they escalate.
Just like we removed barriers for patients with easy-to-use at-home devices, we created a platform with a user-friendly interface, customizable alert settings, and comprehensive care coordination tools. Because healthcare providers have too much to do and not enough time, we built streamlined technology designed to create efficient healthcare workflows.
What is the difference between telehealth and remote patient monitoring?
In short, remote patient monitoring is a specific type of telehealth. However, the term “telehealth” refers to a broad range of services provided remotely via telecommunications technology. “Telehealth” encompasses everything from virtual consultations, doctor visits, mental health counseling, physical therapy, and more. Telehealth enables direct communication between patients and healthcare providers, facilitating diagnosis, consultation, and treatment advice without the need for physical presence.
RPM is a subset of telehealth that involves the collection and analysis of patient health data. This targeted approach focuses on the ongoing monitoring of chronic conditions and preventative health measures, enabling providers to make informed decisions and interventions in real-time.
Does Medicare pay for remote patient monitoring or for remote patient monitoring devices?
Yes, in many cases, Medicare will pay for RPM services and remote patient monitoring devices if the program meets their criteria. Medicare may reimburse providers for RPM services under specific billing codes. This reimbursement policy is meant to encourage the adoption of RPM, as Medicare recognizes how these programs can reduce costs and improve patient outcomes. In our experience at TimeDoc Health, we’ve found our partners typically have an average of $167 per patient, per month in reimbursements.
As of January 1, 2024, Medicare will reimburse Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) for two RPM services under the general care management code G0511 at a rate of $72.98 per patient per month. The services covered include:
- CPT 99454: This covers the use of smart-enabled RPM systems that transmit biometric readings to a digital platform, requiring the patient to transmit at least 16 days of readings within a 30-day period.
- CPT 99457: This reimburses for 20 minutes of clinical staff time spent monitoring and coordinating care for an RPM patient, including live interaction with the patient.
The 2024 expansion of Medicare coverage allows FQHCs and RHCs to bill G0511 multiple times per month for the same patient if the minimum requirements for each subcategory code are met. This flexibility increases the potential for providers to provide enhanced patient care and increase the return on investment for RPM services.
Learn More about Who Qualifies for Remote Patient Monitoring →

Start a Remote Patient Monitoring Program with TimeDoc Health by Your Side
Starting an RPM program can feel overwhelming. However, TimeDoc Health is here to support you every step of the way. The first step is to understand the needs of your patient population and consider how RPM can address those needs. As your partner, we’ll help you leverage our comprehensive RPM solutions, which include:
- Easy to use FDA-approved and FDA-registered devices like cellular-enabled blood glucose meters or blood pressure monitors.
- EHR integrated technology so that data is effortlessly transmitted to your patients’ charts.
Automatic data collection in real-time, allowing you to track patient adherence, program enrollment, and other key insights. - Customizable alert settings to ensure you can address issues quickly for your patients without being overwhelmed by too much data.
- Remote care coordination support from a team of clinically trained TimeDoc Health care managers to serve as an extension of your practice, relieving the administrative burden on your team.
Yes, one of our goals is to help you increase the efficiency of your workflows and provide seamless service to your patients. But our main objective is the same as yours: to make sure that every patient gets the level of care that they deserve—improving health outcomes and patient satisfaction.
Take the first step towards this goal. Get in touch with TimeDoc Health to schedule a live demo today.



