
The healthcare industry is facing a growing challenge.
In the aftermath of the COVID-19 pandemic, providers are still stretched thin, facing staffing shortages and burnout, struggling to offer effective support for people with chronic conditions. And unfortunately, there’s a lot of them: six in ten Americans live with at least one chronic disease like heart disease, cancer, or diabetes. The CDC also reports that these and other chronic diseases are the leading causes of death and disability in America, and are the leading drivers of the nation’s $4.1 trillion in annual health care costs.
With such a major challenge, how can providers possibly begin to address these issues? Remote patient monitoring programs, while not a silver bullet, are gaining popularity due to their effectiveness in addressing patients with chronic conditions. But how does remote patient monitoring work? Is it worth the cost of implementation? What are the potential downsides of these programs?
At TimeDoc Health, we’re here to answer all these questions and more. We’ve put together this guide to remote patient monitoring to help you gain a base of knowledge about these important initiatives and the technology that supports them. Let’s get started.

What is remote patient monitoring?
Remote patient monitoring (RPM), is a beneficial healthcare approach designed to keep doctors connected with their patients’ health status, regardless of the distance between them. It typically involves the use of digital technologies to collect health data from patients in one location and then electronically transmit the information securely to healthcare providers for assessment and recommendations.
The term “remote patient monitoring” is a term that can have many definitions—RPM can also be referred to as remote physiologic monitoring, since you’re monitoring how each patient’s organs function normally. In fact, Medicare uses the term “remote physiologic monitoring” in their coding and billing language. For Medicare, RPM is a set of codes that describes non-face-to-face monitoring and analysis of physiologic factors used to understand a patient’s health status.
At the heart of RPM are devices that are easy to use and designed to monitor a range of health metrics like blood pressure or weight. Collecting this physiological data is just the first step—what really matters is what you do with the information—more on this in a moment.

What are the types of remote patient monitoring devices?
Three of the most common types of RPM devices are blood pressure devices, scales, and blood glucose meters. These three devices are commonly used to manage and monitor chronic conditions, connected via bluetooth or cellular to transmit data to the provider, enabling proactive management of patient health.
The TimeDoc Health team knows how important each of these RPM devices are. Our focus is on providing easy-to-use cellular-enabled devices so that patients can effectively monitor their conditions without barriers. Our straightforward devices don’t need Wi-Fi connectivity or complex setups so even patients who are not tech-savvy can use them. And, on the other side of the equation, we make sure that the data is transmitted securely and directly from our platform onto the patient chart in the EHR (electronic health record). This is an important step to make sure that patient-submitted vitals are automatically updated in the patient’s health record.
Blood Pressure Devices
RPM blood pressure devices enable patients to take regular measurements at home, a vital process for people dealing with conditions like hypertension. The routine flow of data from patient to provider gives the opportunity for immediate interventions if readings fall outside of the patient’s target range, aiding in medication or lifestyle changes to better control high blood pressure.
Scales for Weight Management
The scales used in RPM play a vital role in managing and monitoring conditions like heart disease, obesity, and fluid retention. By providing accurate and timely weight data, these scales help healthcare professionals identify trends, make adjustments to treatment plans, and offer dietary or lifestyle advice to manage weight effectively.
Blood Glucose Meters
Often used by individuals managing diabetes, cellular-enabled blood glucose meters allow for the direct transmission of blood sugar readings to health care providers. This real-time data sharing can help you adjust medications and dietary recommendations in order to maintain optimal glucose levels.
What is remote patient monitoring software?
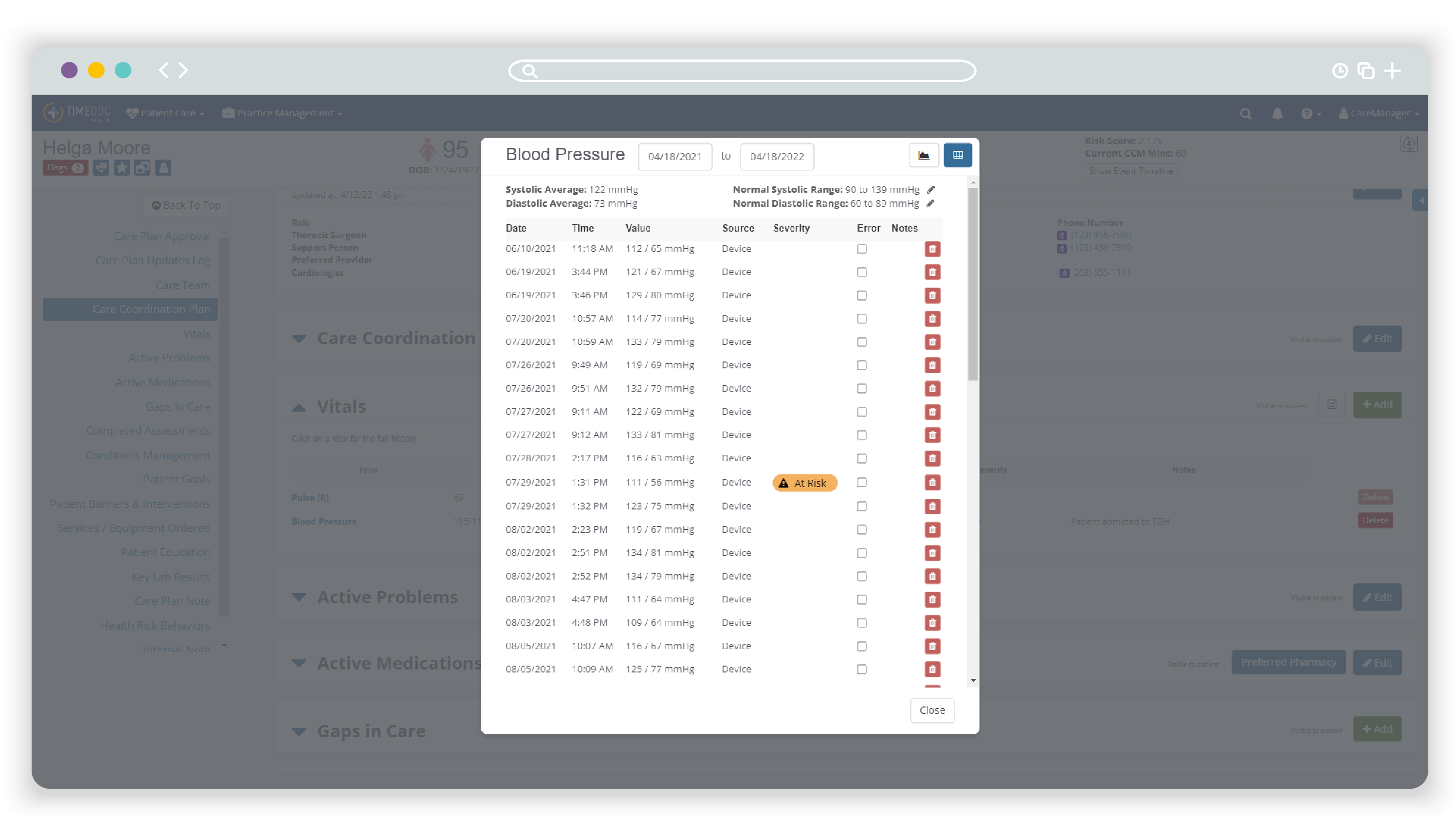
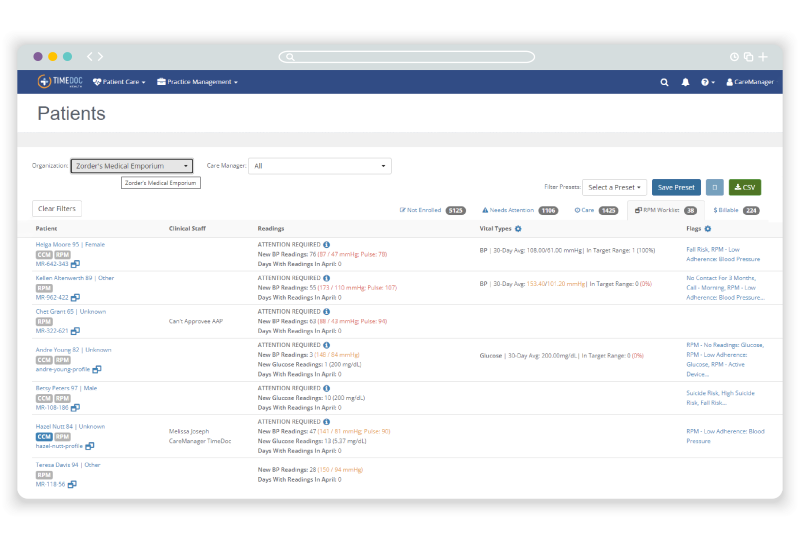
Remote patient monitoring software is any type of technology platform that healthcare providers use to collect and analyze the data that patients submit from their devices at home. At TimeDoc Health, our RPM platform is a prime example of advanced RPM software, designed to integrate seamlessly with existing EHRs. Aside from the collection and transmission of health data between patient and provider, the TimeDoc Health platform plays a crucial role in allowing you to do something with the data you receive.
Our real-time data analytics capabilities trends patient vitals over time and generates alerts for healthcare providers when readings fall outside of a patient’s predefined safe range. This functionality gives you the ability to make data-driven decisions, intervening as necessary to address potential health issues before they escalate.
Just like we removed barriers for patients with easy-to-use at-home devices, we created a platform with a user-friendly interface, customizable alert settings, and comprehensive care coordination tools. Because healthcare providers have too much to do and not enough time, we built streamlined technology designed to create efficient healthcare workflows.
What is the difference between telehealth and remote patient monitoring?
In short, remote patient monitoring is a specific type of telehealth. However, the term “telehealth” refers to a broad range of services provided remotely via telecommunications technology. “Telehealth” encompasses everything from virtual consultations, doctor visits, mental health counseling, physical therapy, and more. Telehealth enables direct communication between patients and healthcare providers, facilitating diagnosis, consultation, and treatment advice without the need for physical presence.
RPM is a subset of telehealth that involves the collection and analysis of patient health data. This targeted approach focuses on the ongoing monitoring of chronic conditions and preventative health measures, enabling providers to make informed decisions and interventions in real-time.

What does remote patient monitoring do?
RPM enables a continuous loop of monitoring that helps shift the paradigm from reactive care to proactive care. Ultimately, the impact of RPM includes:
- Patient Engagement and Empowerment: RPM engages patients by providing them with the tools to actively monitor their health. This approach helps individuals understand their conditions better and fosters a sense of control over their health outcomes.
- Early Detection and Prevention: With continuous monitoring, providers are able to establish a baseline and set alerts if symptoms fall outside of the normal range. By catching abnormal symptoms early, healthcare providers can intervene sooner, preventing conditions from worsening.
- Reduced Hospitalizations and Emergency Visits: Due to early interventions, patients can often manage their condition effectively at home. This can lead to fewer hospital stays and emergency visits, ultimately improving patient quality of life and reducing healthcare costs for both patients and providers.
- Improved Medication Compliance: RPM can improve medication adherence by reminding patients to take their medicine and allowing providers to check if treatments are followed correctly through data monitoring.
- Optimized Resource Allocation: By understanding who needs immediate attention through real-time data, providers can allocate resources more efficiently, enhancing the overall quality of care.
What are the benefits of RPM?
In addition to the benefits listed above, RPM serves a dual-purpose role in the healthcare ecosystem, benefiting both patients and healthcare providers. The benefits of remote patient monitoring result in improved outcomes for patients and greater efficiency for providers.
From the Patient Perspective
RPM empowers patients to take an active role in their healthcare journey from the comfort of their own home. They are given the tools and support needed to monitor their health closely. By having their health data collected and analyzed regularly, patients can receive timely feedback and interventions from their healthcare providers, reducing the likelihood of health deteriorations that lead to ER visits.
For patients with mobility issues or those who live in remote areas, RPM can provide high-quality care in an accessible way. This convenience can have a significant positive impact on patients engaging with and adhering to their healthcare plans.
Patients also have oversight from their providers who can advise them to seek emergency care if the situation warrants it. Life with a chronic health condition can be difficult and scary—RPM can enhance patient quality of life and instill a sense of security and empowerment, since they know their health is being watched over without stepping into a doctor’s office.
From the Provider Perspective
For healthcare providers, RPM offers efficient technology tools that integrate seamlessly into their existing healthcare systems. With the capability to monitor patients remotely, providers can identify potential health issues before they escalate, improving patient outcomes, enhancing the efficiency of healthcare delivery, and optimizing resource utilization within healthcare facilities.
In addition, RPM systems are scalable, making it easier for healthcare providers to expand their services as needed without significant additional costs. With modern technology platforms like that offered by TimeDoc Health, it is increasingly feasible to manage a large patient population effectively—a crucial ability in the face of growing healthcare demands.
The wealth of data collected through RPM devices gives healthcare providers the ability to make more informed decisions. This data-driven approach can lead to personalized treatment plans based on the specific needs and responses of each patient, enhancing the overall effectiveness of medical interventions.
Overall, RPM represents a significant shift towards more accessible, efficient, and proactive healthcare. By leveraging technology to bridge the gap between patients and providers, RPM programs with active participation ensures that timely, data-driven decisions can be made, leading to better health outcomes and a more responsive healthcare ecosystem.
What are the disadvantages of RPM?
One of the primary disadvantages of remote patient monitoring programs is the fact that both patients and providers must be actively participating in order for it to be effective.
From the Patient Perspective
Patients must consistently use the monitoring devices correctly and engage with their healthcare providers. This requirement can be challenging, especially for elderly patients or those who struggle to use technology. Additionally, this active participation necessitates a level of commitment and discipline to adhere to the monitoring schedule. This may be burdensome for some patients, potentially leading to inconsistent data transmission and gaps in monitoring.
Moreover, since the success of RPM is contingent on patients having access to the necessary technology and a stable, reliable way to transmit that data, individuals in rural areas or from lower socioeconomic backgrounds may not have reliable access to these technologies, potentially limiting the effectiveness of RPM for these populations.
From the Provider Perspective
Providers also play a critical role in the success of RPM programs and must be actively engaging with the technology and responding to patient data and alerts. This engagement means providers must take the time out of their busy schedules to familiarize themselves with the RPM software, understand how to interpret data from various devices, and then integrate this information into patient care plans effectively. This includes navigating patient dashboards, setting appropriate alert thresholds, and responding to alerts in a timely fashion.
Moreover, the effectiveness of RPM hinges on providers not ignoring alerts generated by the monitoring systems. These alerts are designed to flag potential health issues or deviations from normal health parameters. Providers must establish protocols for responding to alerts, ensuring that each is assessed and addressed appropriately to maintain the integrity of the RPM program and deliver proactive patient care.
These disadvantages are not insurmountable. The key to success is educating patients and providers on why RPM is so important and encouraging active participation from both sides. Finding the right RPM partner with easy-to-use devices and technology and a team who can provide support to the healthcare provider is vital. With nearly a decade of experience implementing RPM programs, our team is deeply committed to helping you succeed.
What is a remote patient monitoring example?
Remote patient monitoring programs are experienced by both patients and healthcare providers. Let’s take a look at “Alex,” a 70-year-old Puerto Rican man with hypertension and coronary artery disease, and his healthcare team, to illustrate the transformative impact of RPM.
From Alex’s Perspective:
Before RPM, Alex faced several barriers to managing his health effectively, including language barriers, low literacy, and limited access to healthcare technology. Despite in-person visits and the inclusion of a Spanish interpreter, Alex’s blood pressure remained uncontrolled—a common challenge for patients with chronic conditions. When the healthcare provider partnered with TimeDoc Health, the RPM program marked a turning point. Equipped with a cellular-enabled blood pressure monitor (and a Spanish-speaking TimeDoc care coordinator), Alex began transmitting daily health data directly to his care team. This constant flow of information allowed his providers to adjust his medication in real-time, leading to dramatically improved blood pressure control. For Alex, RPM wasn’t just a new tech tool—it was a lifeline, offering not just a better health outcome but a deeper sense of engagement and empowerment in managing his conditions.
From the Healthcare Provider’s Perspective:
Alex’s healthcare team encountered their own set of challenges, chief among them the pressure of delivering comprehensive care within the constraints of limited time and resources. IMplementing RPM required the team to navigate new technologies, integrating them into their existing workflows without exacerbating clinician burnout. With the help of TimeDoc’s care team, they discovered the power of RPM to:
- Boost Alex’s engagement and satisfaction with his care plan. Removing the barrier of language was important, as well as giving him the opportunity to participate in his own health management.
- Improve Alex’s outcomes. He started following his medication schedule more diligently since he could now see the clear correlation between taking his medication consistently and his home blood pressure readings. Frequent telephone calls from his Spanish-speaking care manager reinforced the importance of taking his medication and blood pressure readings consistently.
- Reduce the administrative burden on the healthcare team. With easy-to-access clinical data in the TimeDoc platform, the provider could find critical patient data quickly and make data-based decisions in real-time. With the support of TimeDoc’s care manager team, the provider didn’t have to dedicate time to the administrative tasks like calling Alex frequently to remind him to take his medication and blood pressure readings, ensuring that there weren’t major gaps in monitoring.
Alex and his healthcare team is just one of the many examples of remote patient monitoring programs and how this comprehensive approach benefits all stakeholders in a patient’s healthcare journey. For patients, RPM offers a means to actively participate in their health management, fostering better outcomes and greater satisfaction. For providers, it provides a suite of efficient technology tools that enhance patient care and operational efficiency.
Read more about “Alex’s” story and how RPM played an important role.
How much does RPM cost?
The cost of implementing and maintaining an RPM program will vary significantly, with yearly expenses per patient ranging from a few hundred dollars to upwards of $5,000+. Because there are so many variables, it’s difficult to put an exact answer. A better way to ask this question is: Is remote patient monitoring worth it? We certainly think so. Let’s look at high blood pressure for a moment:
- Nearly 1 in 2 US adults (116 million) has high blood pressure, and most of them (92 million) may need to both change their lifestyle and take prescription medicine.
- About 3 in 4 US adults with high blood pressure (92 million) don’t have it under control (defined as blood pressure less than 130/80 mm Hg)
- The CDC reports that using team-based care that includes a pharmacist could prevent up to 91,900 heart attacks, 139,000 strokes, and 115,400 cardiovascular deaths over 5 years among US adults with uncontrolled high blood pressure.
- The NIH reports that 48% of adults have high blood pressure, with direct costs in excess of $130 billion per year.
There’s clearly a problem here. But is remote patient monitoring effective when treating high blood pressure? The answer is yes. NIH’s study of RPM intervention found it was effective at increasing blood pressure control and decreasing systolic blood pressure at 90 days after implementation. Additionally, they found that the comprehensive RPM program was able to significantly reduce office-based visits during the study period and was financially feasible and cost-effective.
Let’s zoom out a bit and consider statistics like:
- The University of Pittsburgh Medical Center reduced the risk of hospital readmissions by 76% through the use of RPM.
- A survey of 25 healthcare organizations with RPM programs found that 38% reported reduced admissions and 17% cited cost reductions.
- Our internal data here at TimeDoc Health has shown that the healthcare providers we partner with have experienced 15% improvement in blood pressure control and 90% patient retention in Virtual Care Management programs.
These are just a few statistics, but over and over again, the results are the same: a properly implemented RPM program can have major benefits for patients and providers. As you consider the full picture—how RPM can improve patient outcomes and reduce costs for providers—the question becomes, can you afford NOT to implement an RPM program?
Does Medicare pay for remote patient monitoring? Does Medicare pay for remote patient monitoring devices?
In many cases, Medicare will pay for RPM services and remote patient monitoring devices if the program meets their criteria. Medicare may reimburse providers for RPM services under specific billing codes. This reimbursement policy is meant to encourage the adoption of RPM, as Medicare recognizes how these programs can reduce costs and improve patient outcomes. In our experience at TimeDoc Health, we’ve found our partners typically have an average of $167 per patient, per month in reimbursements.

How do I start a remote patient monitoring program? With TimeDoc Health by your Side
Starting an RPM program can feel overwhelming. However, TimeDoc Health is here to support you every step of the way. The first step is to understand the needs of your patient population and consider how RPM can address those needs. As your partner, we’ll help you leverage our comprehensive RPM solutions, which include:
- Easy to use FDA-approved and FDA-registered devices like cellular-enabled blood glucose meters or blood pressure monitors.
- EHR integrated technology so that data is effortlessly transmitted to your patients’ charts.
Automatic data collection in real-time, allowing you to track patient adherence, program enrollment, and other key insights. - Customizable alert settings to ensure you can address issues quickly for your patients without being overwhelmed by too much data.
- Remote care coordination support from a team of clinically trained TimeDoc Health care managers to serve as an extension of your practice, relieving the administrative burden on your team.
Yes, one of our goals is to help you increase the efficiency of your workflows and provide seamless service to your patients. But our main objective is the same as yours: to make sure that every patient gets the level of care that they deserve—improving health outcomes and patient satisfaction.
Take the first step towards this goal. Get in touch with TimeDoc Health to schedule a live demo today.
